 Congenital uterine malformations (CUM) are deviations from normal anatomy resulting from incorrect embryological development. 5.5% of women are affected if we consider the general population, 8.0% of infertile women, 13.3% if we consider women with a history of spontaneous abortions and 24.5% considering those with previous miscarriages and infertility.
Congenital uterine malformations (CUM) are deviations from normal anatomy resulting from incorrect embryological development. 5.5% of women are affected if we consider the general population, 8.0% of infertile women, 13.3% if we consider women with a history of spontaneous abortions and 24.5% considering those with previous miscarriages and infertility.
Although most women are asymptomatic, it is possible, based on the defect they are suffering from, to identify different types of symptoms. Obstructive abnormalities can lead to symptoms such as: primary amenorrhea (absence of the first menstruation), recurrent pelvic pain, progressive dysmenorrhea, presence of pelvic mass. Non-obstructive uterine abnormalities (for example, septate uterus and the T-shaped uterus) are more likely to be related to infertility and pregnancy complications; sometimes they begin with dyspareunia (pain during sexual intercourse) as in the case of longitudinal vaginal septa.
Complete and partial uterine septum appear to have the worst reproductive outcomes, with a reduced conception rate, an increased risk of spontaneous abortion in the first trimester, and fetal malpresentation at delivery.
Unification defects (bicornuate and unicornuate uterus) do not appear to reduce fertility, while they are associated with an increased risk of adverse outcomes during pregnancy.
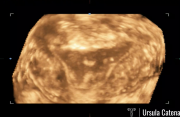
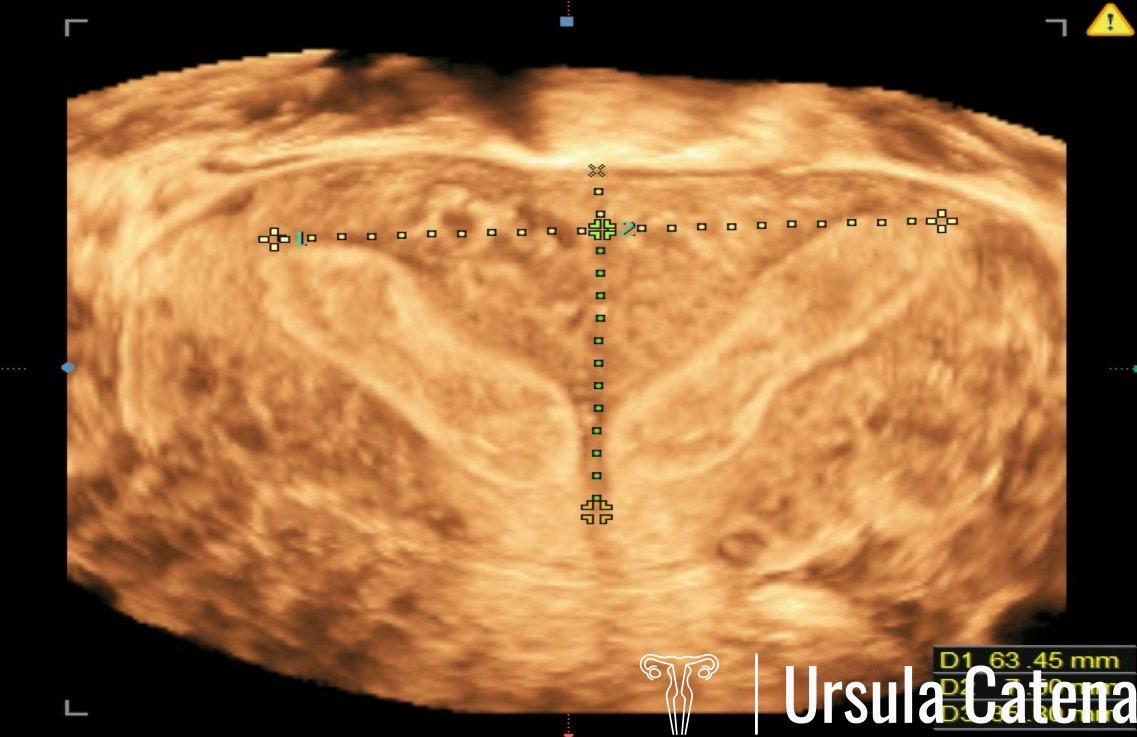
Three-dimensional (3D) ultrasound has become the non-invasive gold standard method for a correct diagnosis of uterine malformations, because it provides a clear image of the internal and external contours of the uterus and makes the evaluation of uterine morphology more reproducible, thanks to the possibility to obtain reproducible and comparable measurements, as well as being less invasive than other commonly used radiological and surgical diagnostic modalities (magnetic resonance, laparoscopy).
Studies have also been published that report a beneficial effect of hysteroscopic metroplasty even in women with a T-shaped uterus with a history of infertility and/or recurrent abortion, with an exceptionally high rate of live birth rate. T-shaped uterus hysteroscopic tratment is a safe and effective method to implement reproductive outcomes, with an increase in the live birth rate and a reduction in the miscarriage rate.
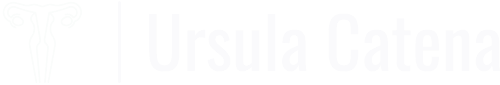
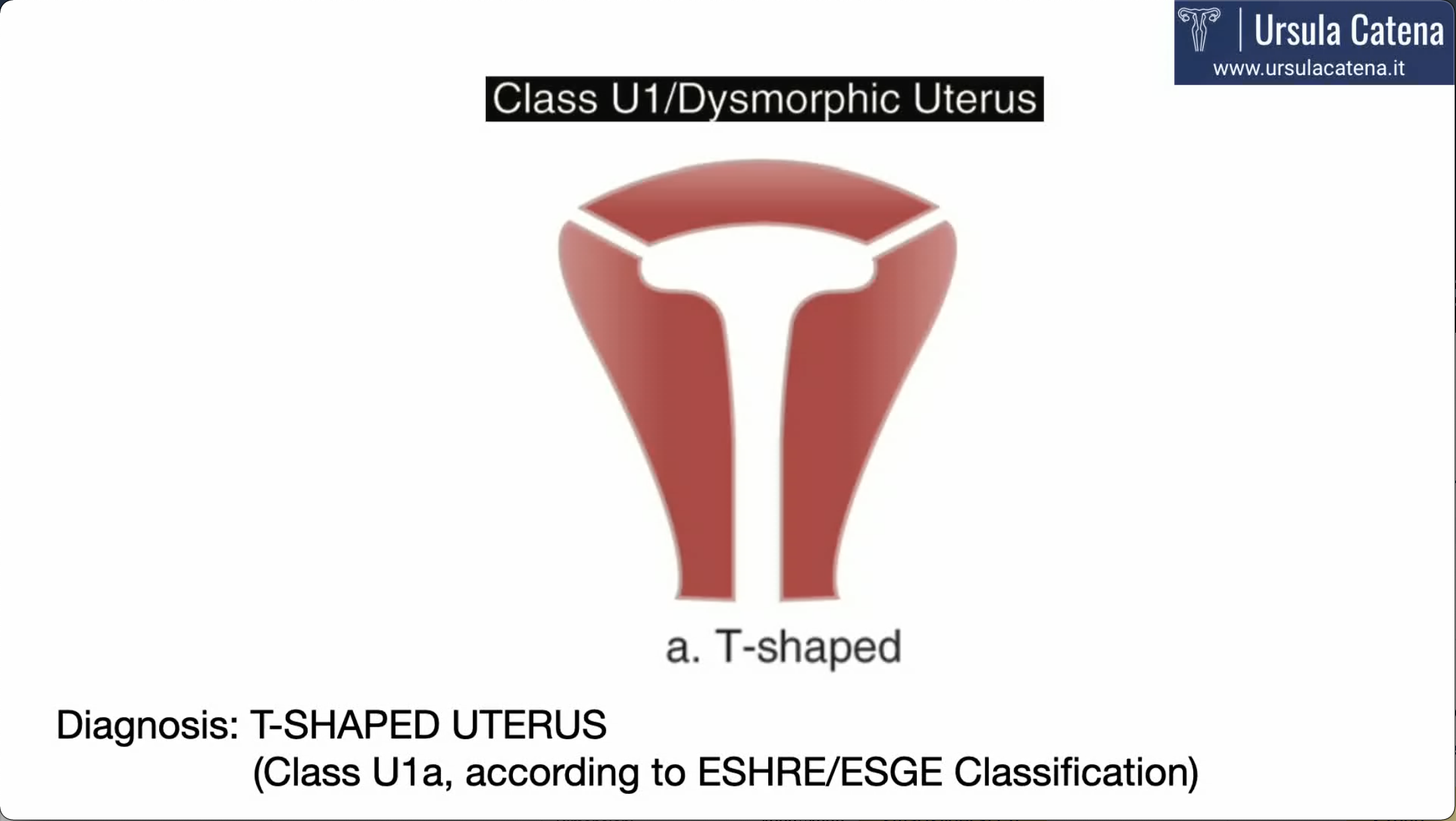
In recent decades, many classifications have been published. Currently one of the most used classifications is the ESHRE/ESGE classification of 2013 through which all malformations of the female genital tract can be easily categorized.
Among the indications for surgery there are primarily obstructive anomalies, aimed at resolving the symptoms of dysmenorrhea, chronic pelvic pain and preventing further repercussions on the reproductive organs. While an unicornuate uterus does not justify surgery, the presence of rudimentary "functioning" horns, often associated with the unicornuate uterus, require surgical removal to prevent the risk of hematometra (collection of blood in the uterine cavity) or the onset of pregnancy in the rudimentary horn (if the horn communicates with the other cavity).
In case of fusion or unification defects, as in the case of uterine septum, the Italian Society of Gynecological Endoscopy (SEGI) recommends hysteroscopic treatment as it improves the live birth rate (level of evidence V, strength of recommendation B) ( SEGI, 2015).
Surely the uterine septum remains the most common uterine malformation and some authors have reported an effective and safe treatment for this pathology even in an "office" setting.
Treatment of partial septate uterus remains a very controversial topic.
Therefore, hysteroscopic resection of a uterine septum may be offered on an individualized basis to women with a history of recurrent infertility and/or abortion by experienced surgeons in specialized centers, while the treatment of an accidentally diagnosed partial septum may be questionable and unproven.
The change that we can observe over time regarding indications and actual clinical practice is very evident: the increasing availability of less invasive surgical approaches has made possible a greater application of these techniques, which is increasingly based on the consideration of future reproductive options for woman and that allow patient herself to be involved in this decision-making process. Furthermore, the need to perform hysteroscopic metroplasty only in dedicated centers with experts trained in the management of complex Uterine Malformations is generally shared. Obviously, surgeons who operate in high-volume centers with centralized care - for example 50-100 women with septate uterus per year - can certainly have better results than surgeons who operate in low-volume centers.
UTERINE SEPTUM: DIAGNOSIS AND TREATMENT
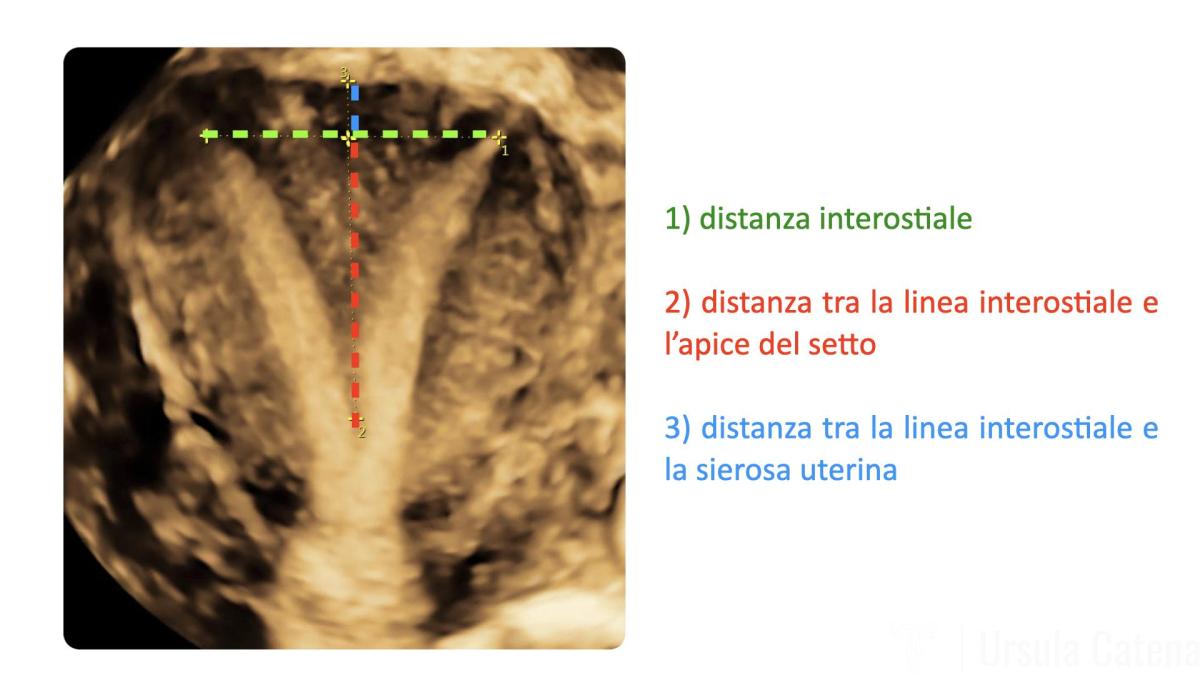
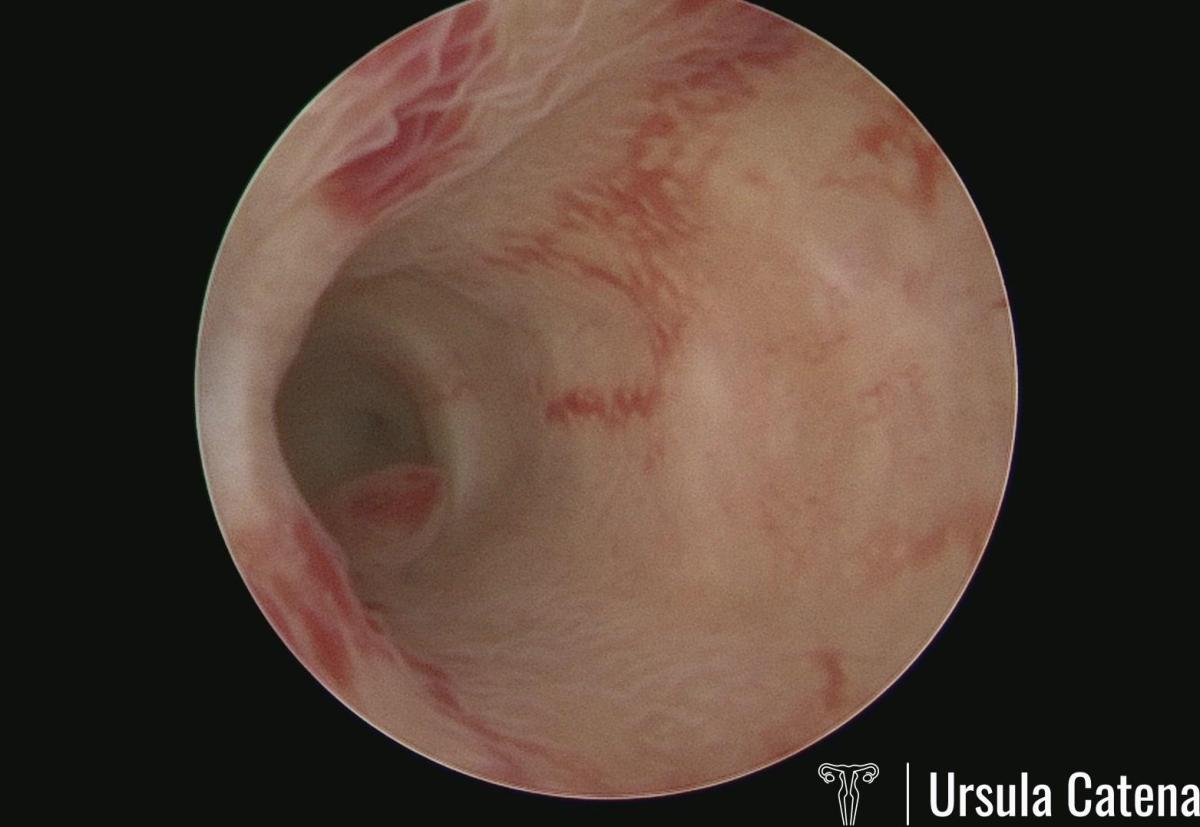
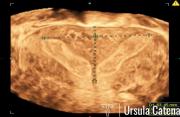
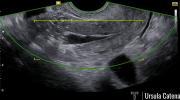
In the event of a suspected uterine septum, at the CLASS Hysteroscopy center, patient first of all undergoes a 3D ultrasound and office diagnostic hysteroscopy.
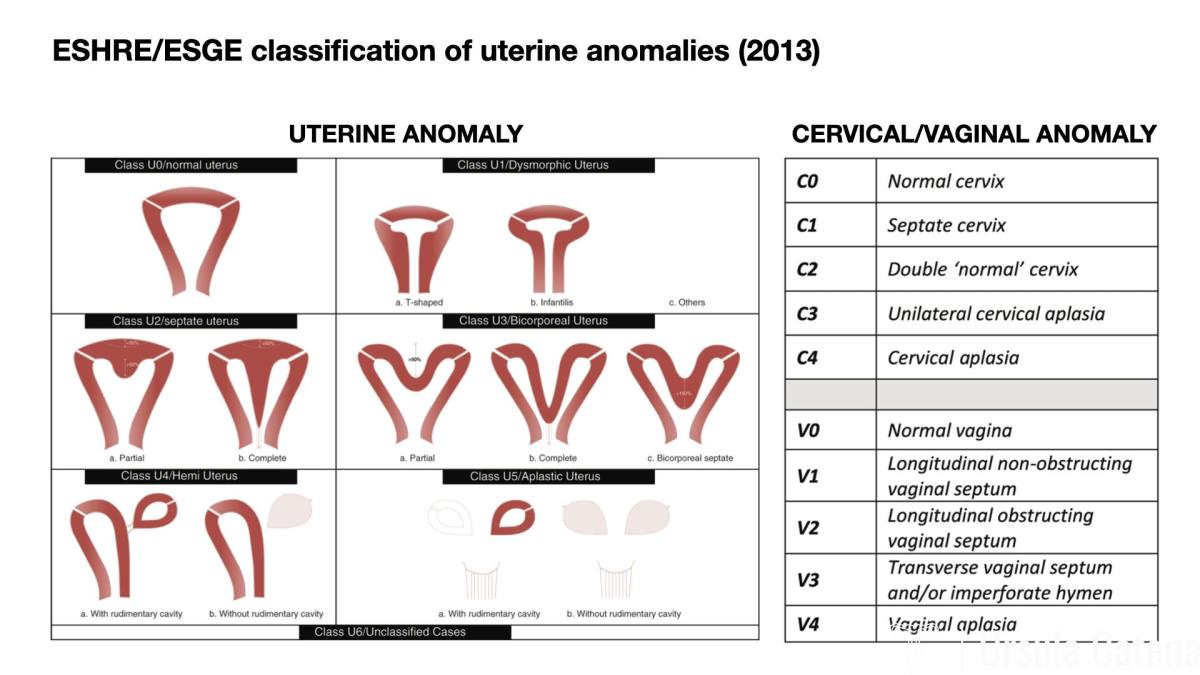
During 3D ultrasound examination, the following will be evaluated: 1) interostial distance; 2) distance between the interostial line and the apex of the septum; 3) distance between the interostial line and the uterine serosa.
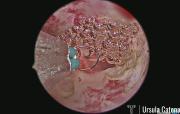
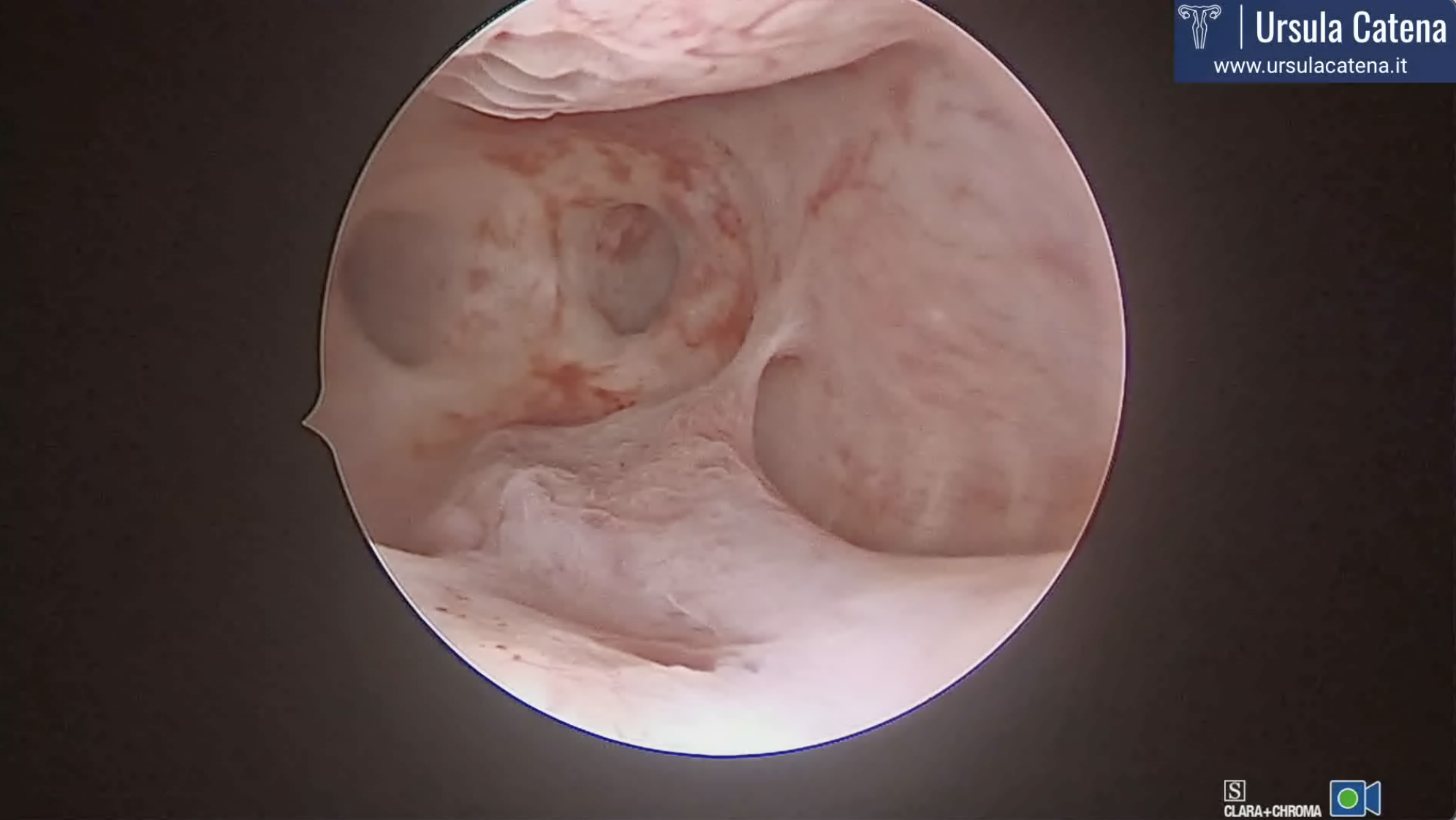
Office diagnostic hysteroscopy will allow us to confirm the ultrasound diagnosis and to exclude other associated anomalies (for example, any associated malformations of the cervix and/or vagina).
Once the diagnosis of certainty has been reached and discussed with patient the therapeutic options based on her medical history (possible infertility and/or previous miscarriages), she will be advised to start oral therapy based on progestin or estrogen-progestin in order to prepare the endometrium for surgery. Therapy must be started from the first day of the next menstrual cycle and taken every day except for different indications from the doctor. The menstrual cycle may not occur and the onset of spotting (small blood loss) will be possible during therapy.
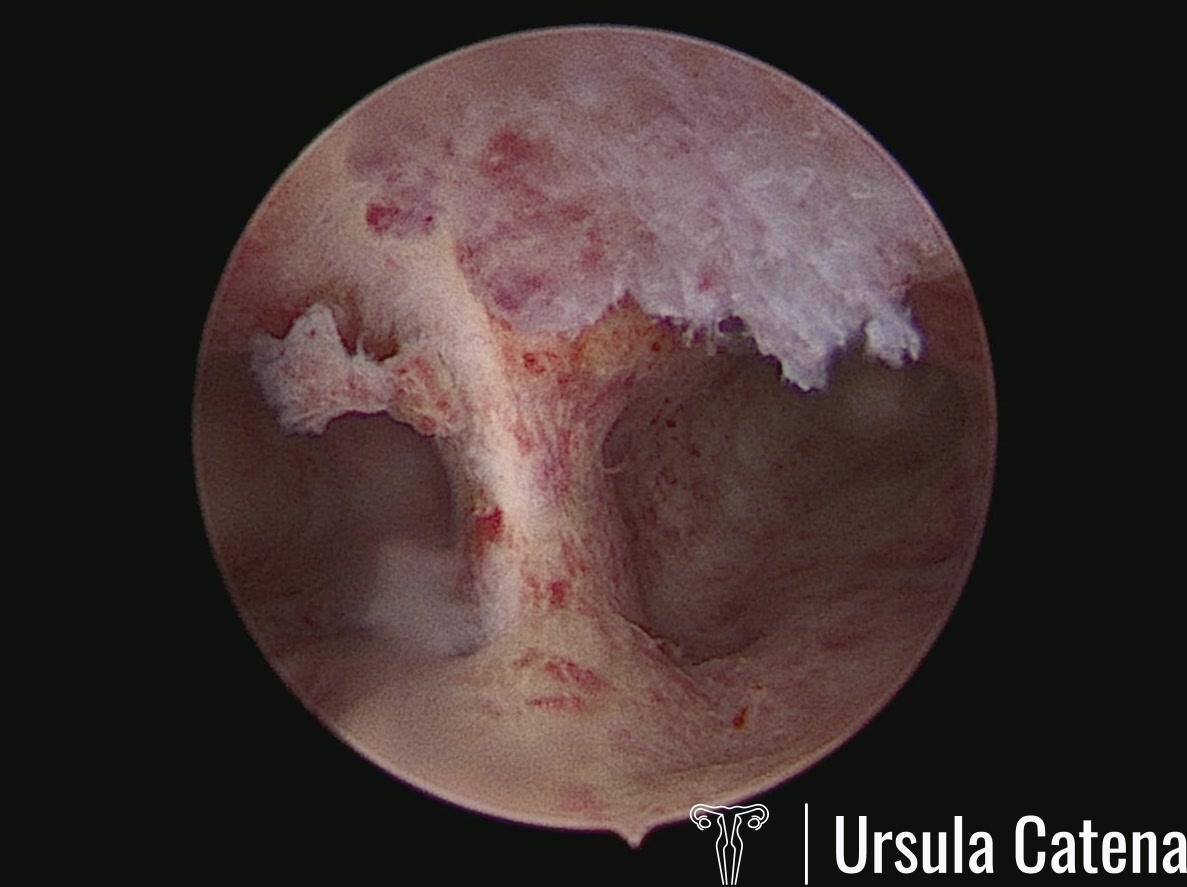
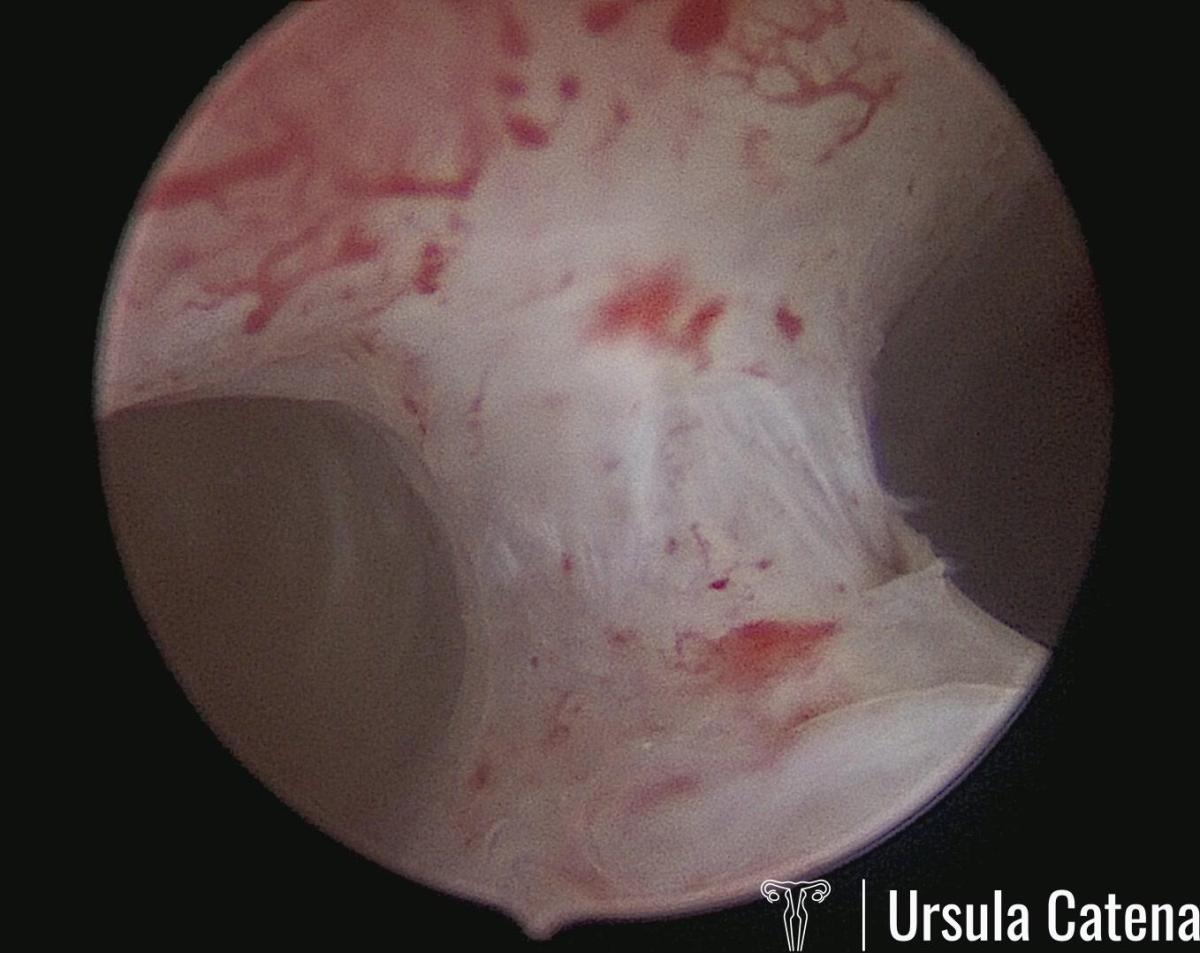
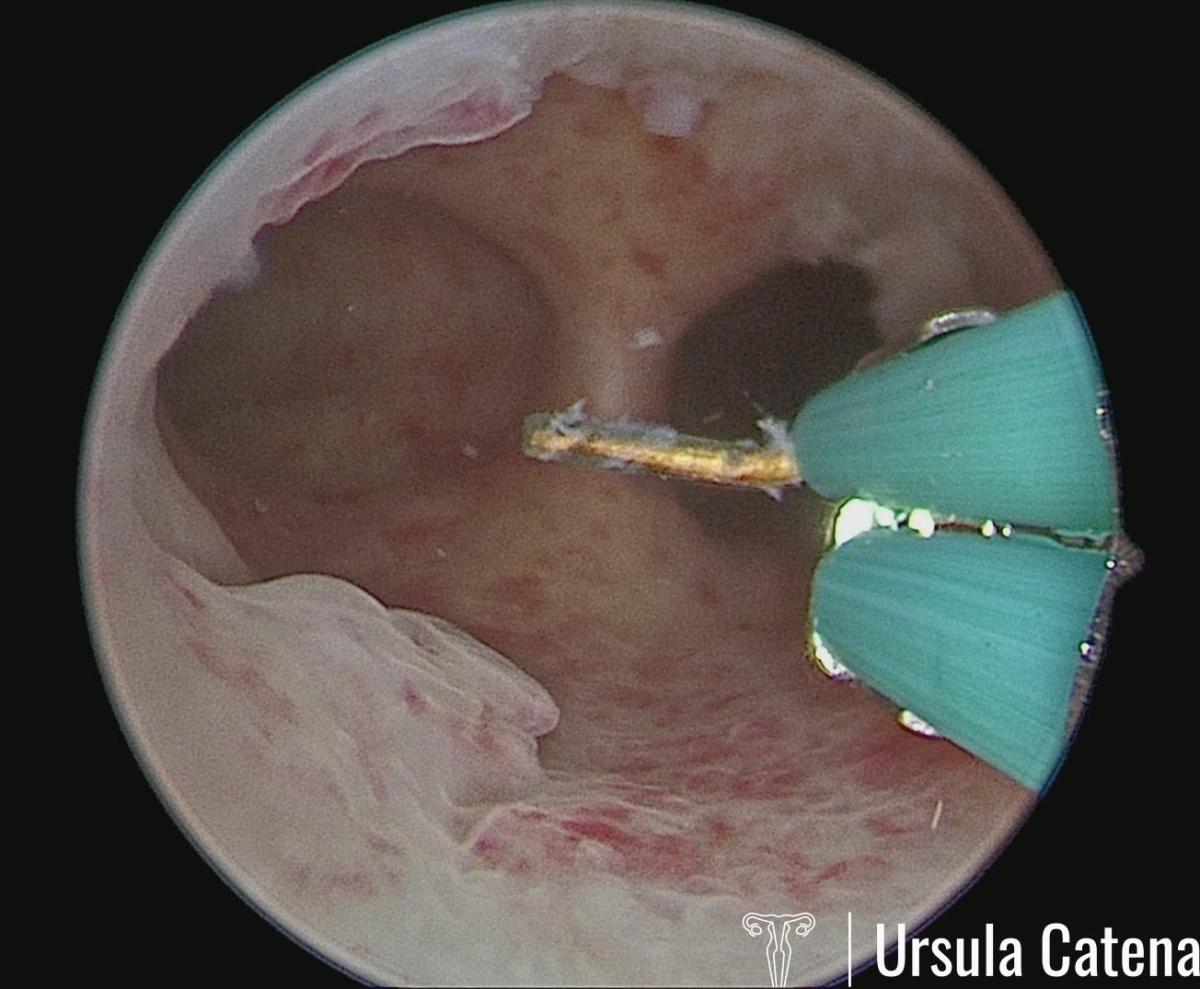
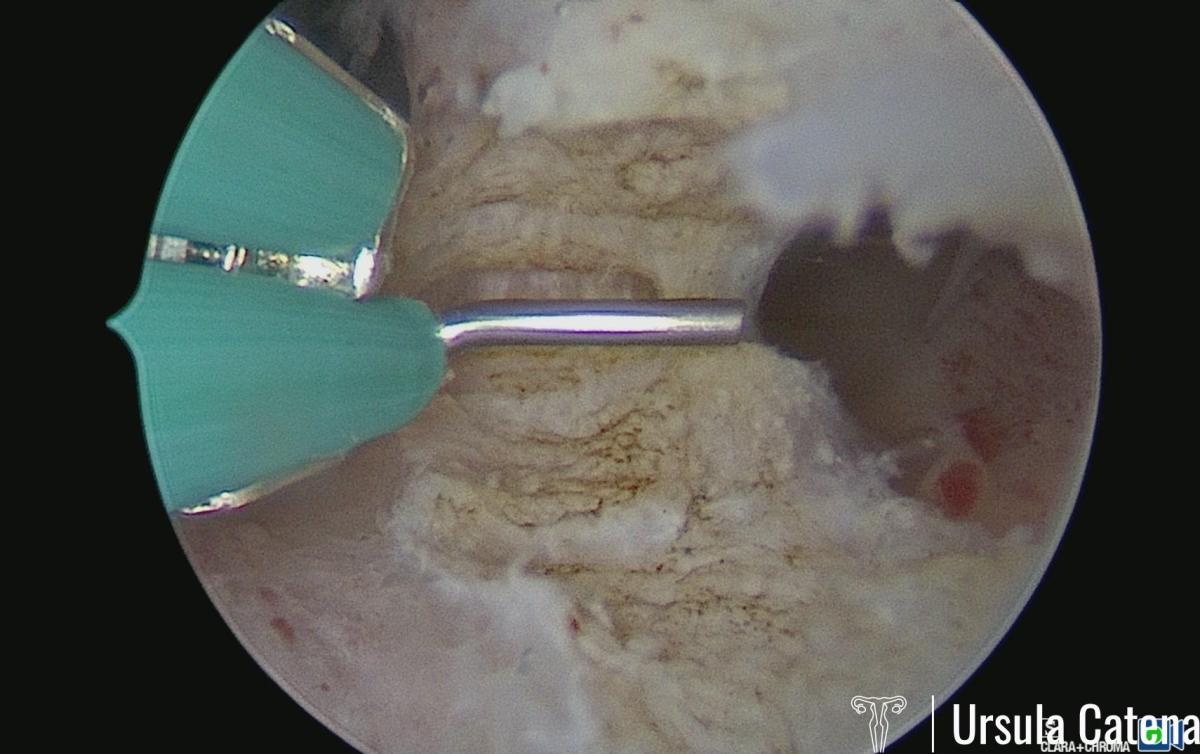
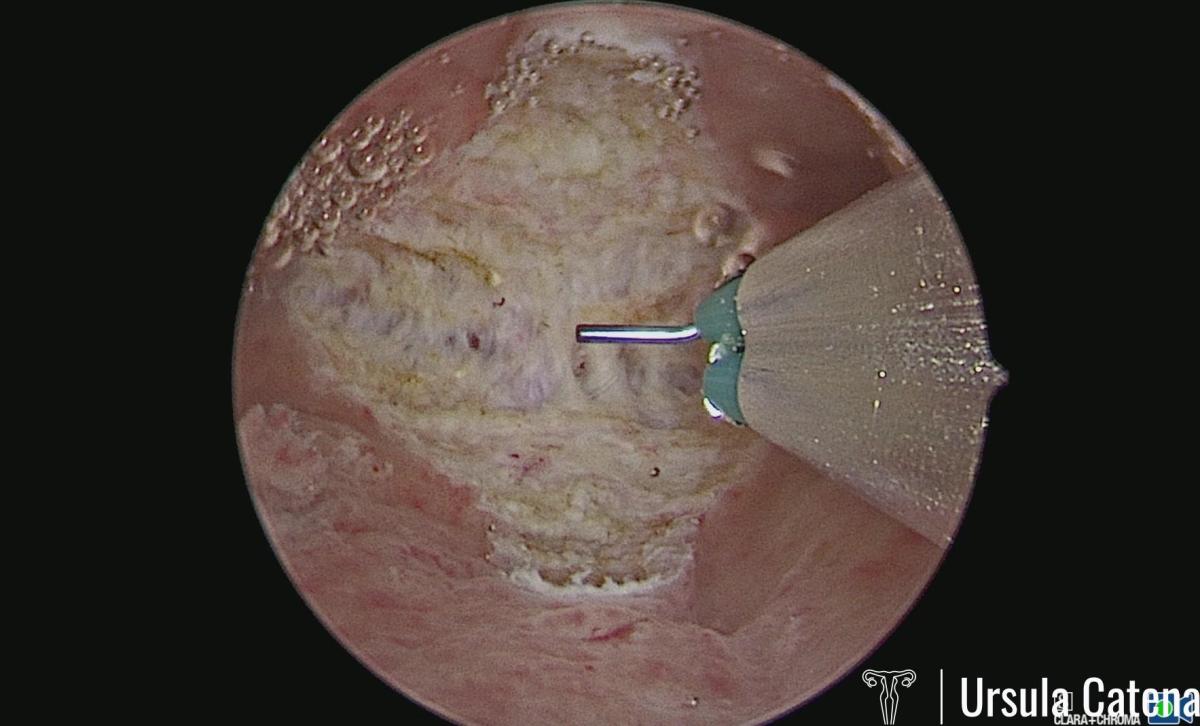
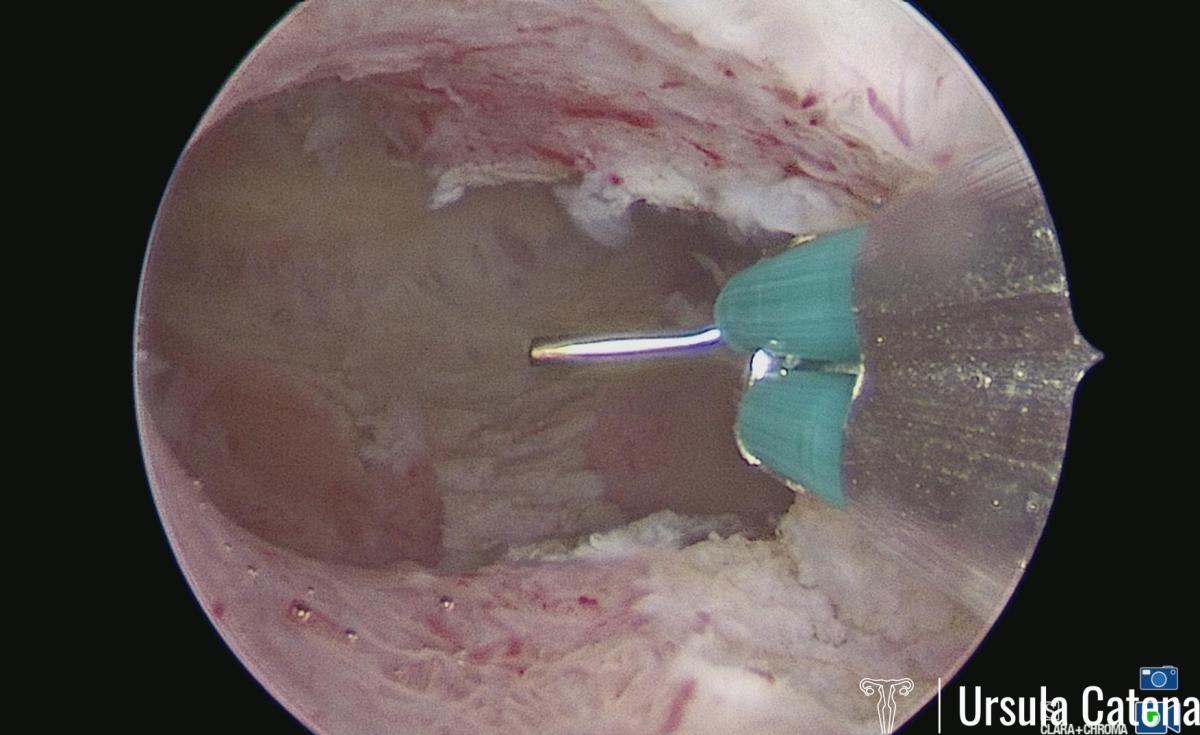
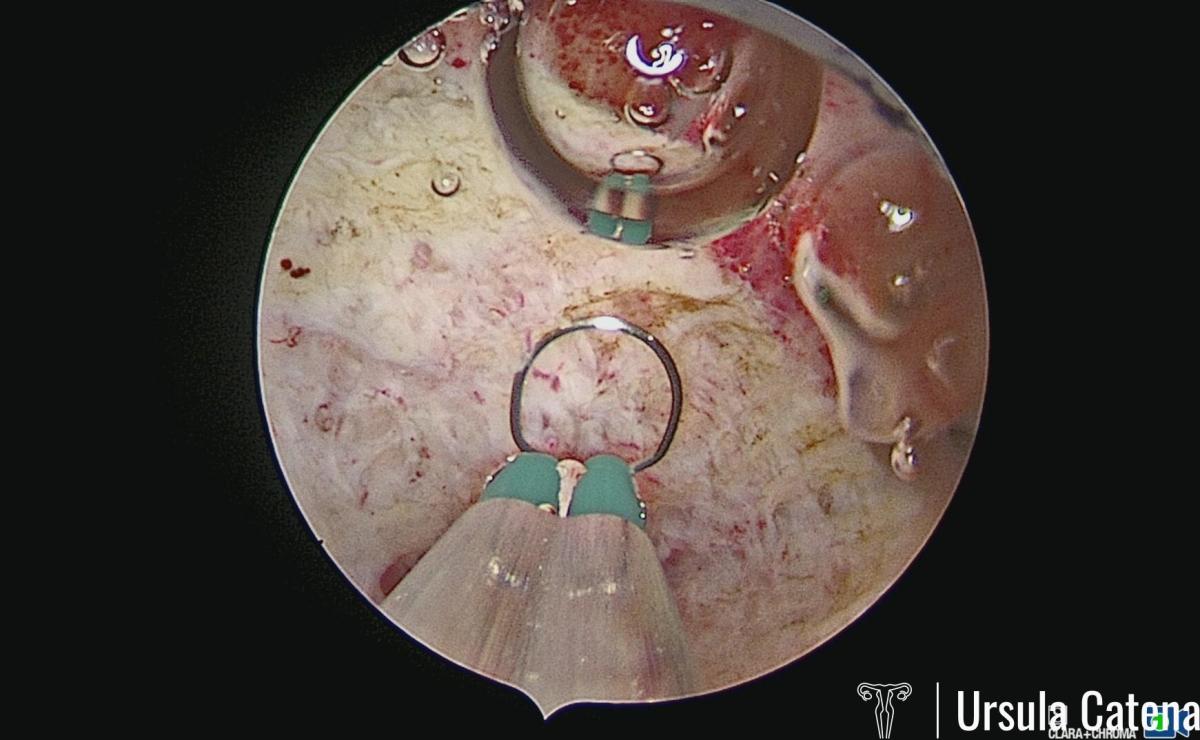
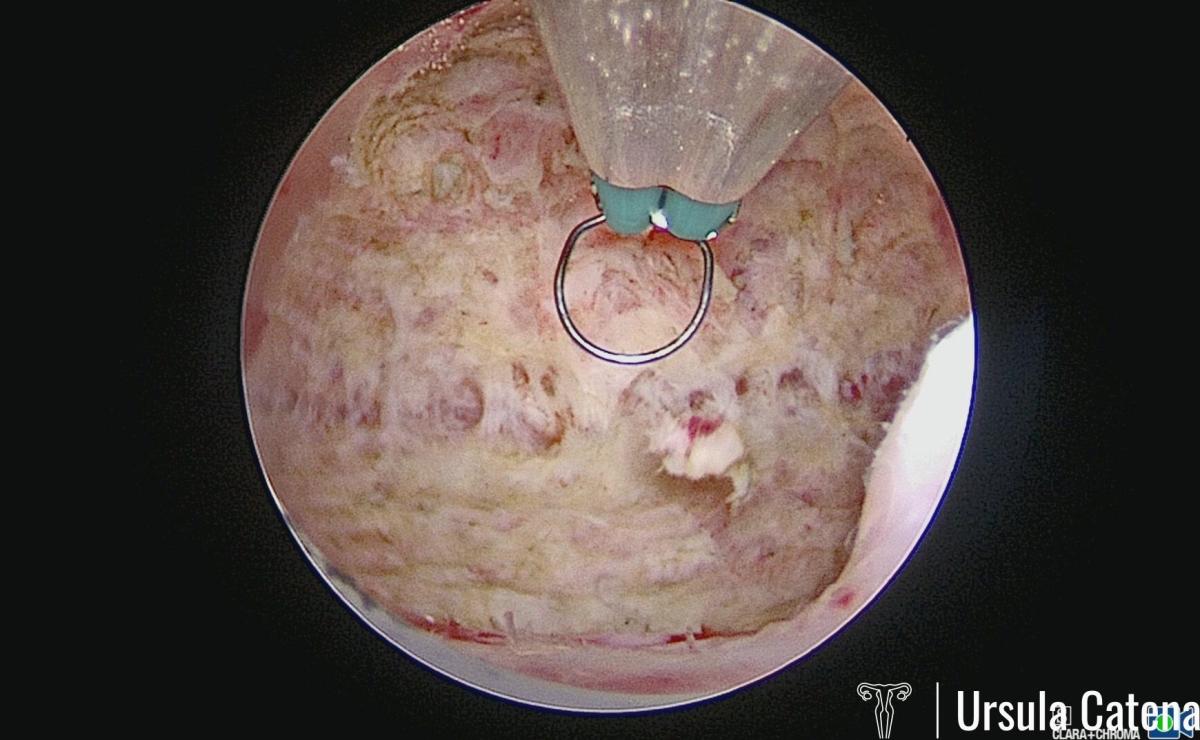
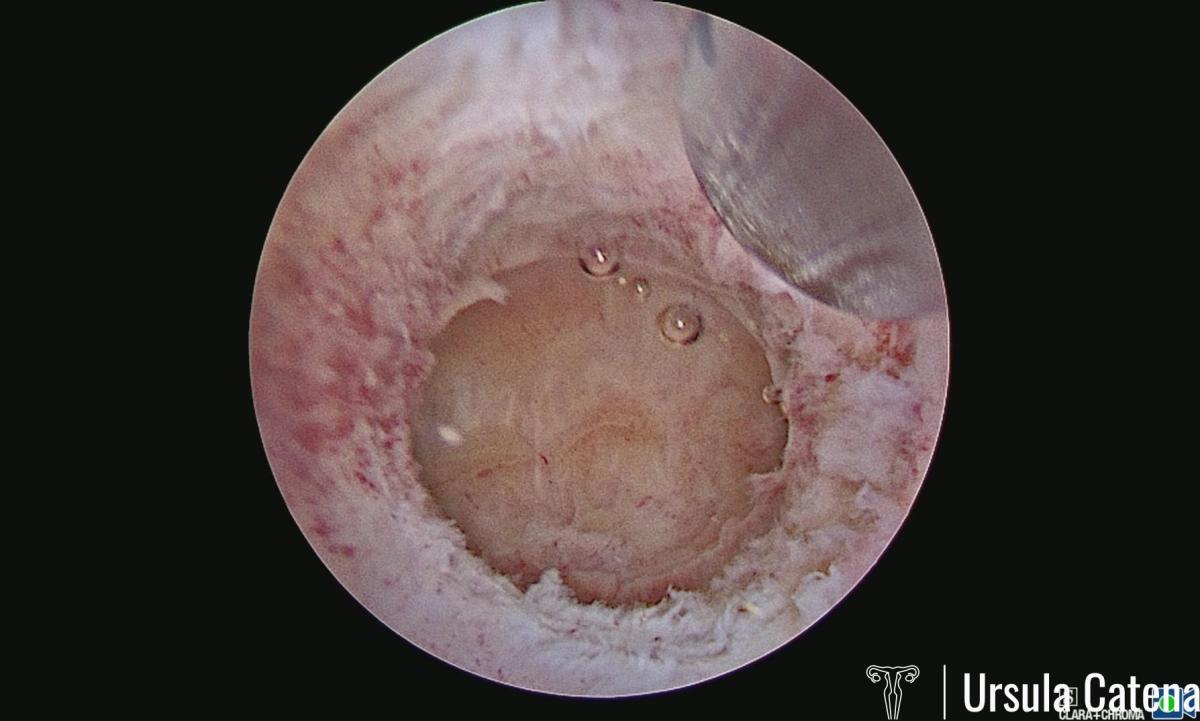
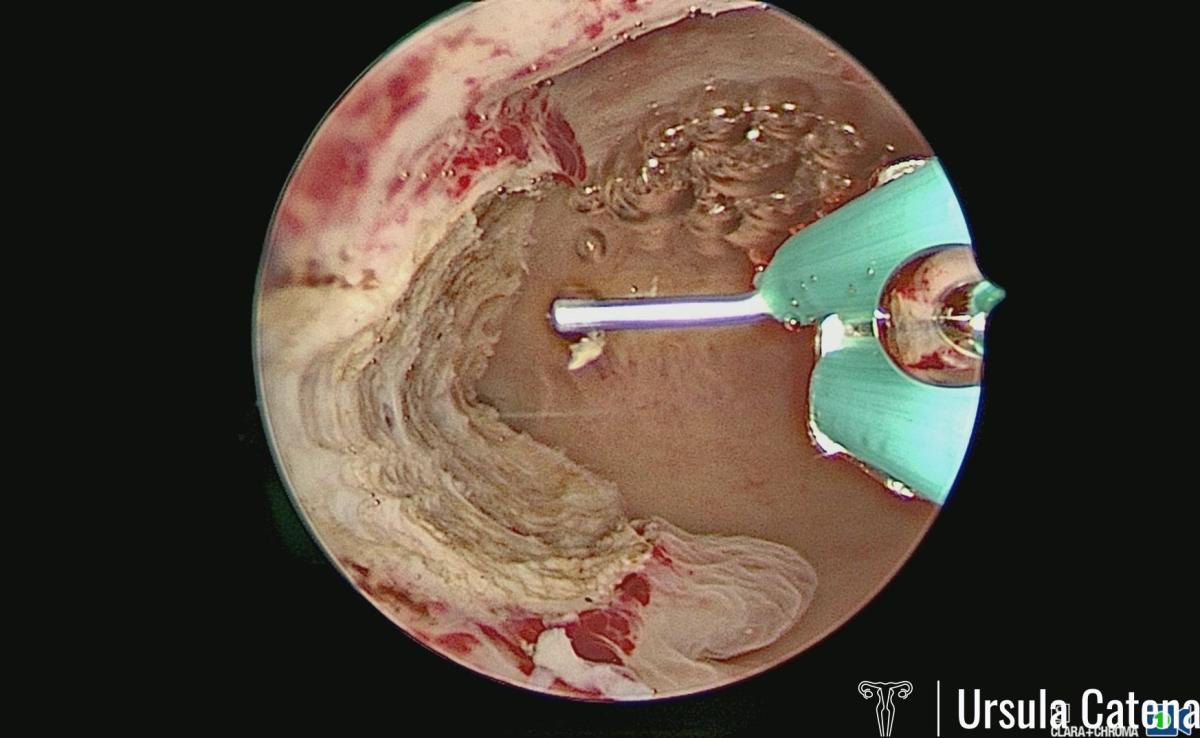
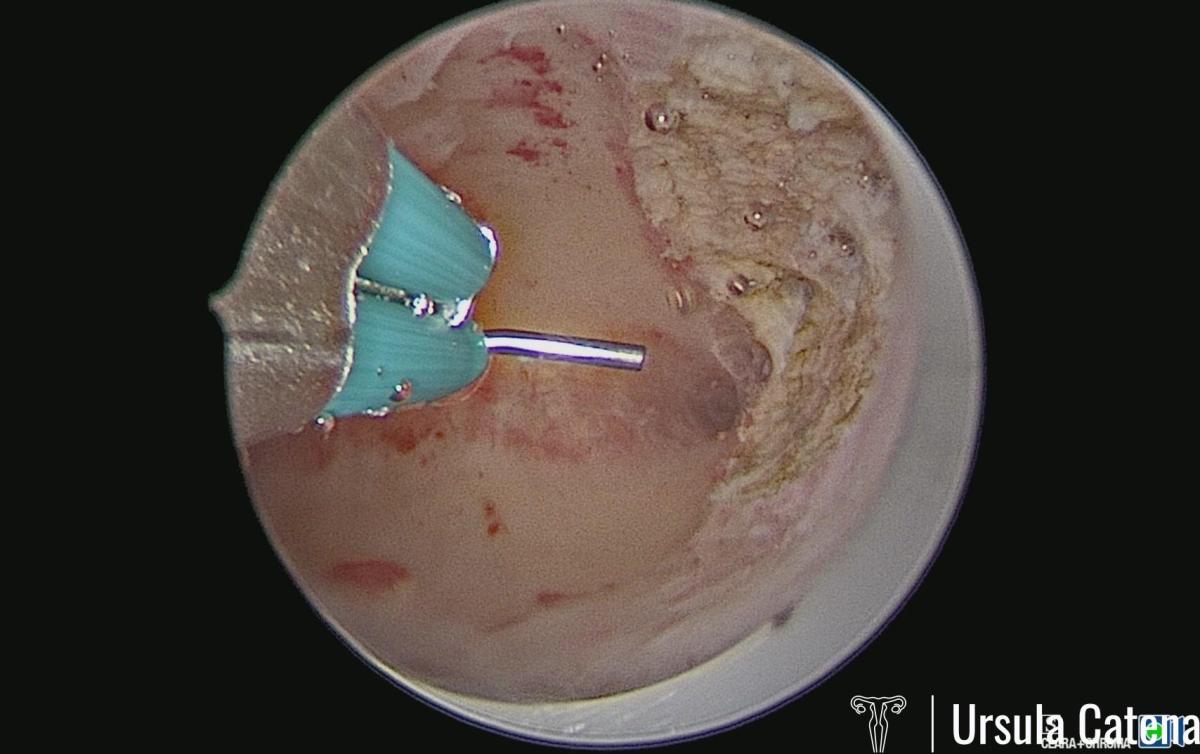
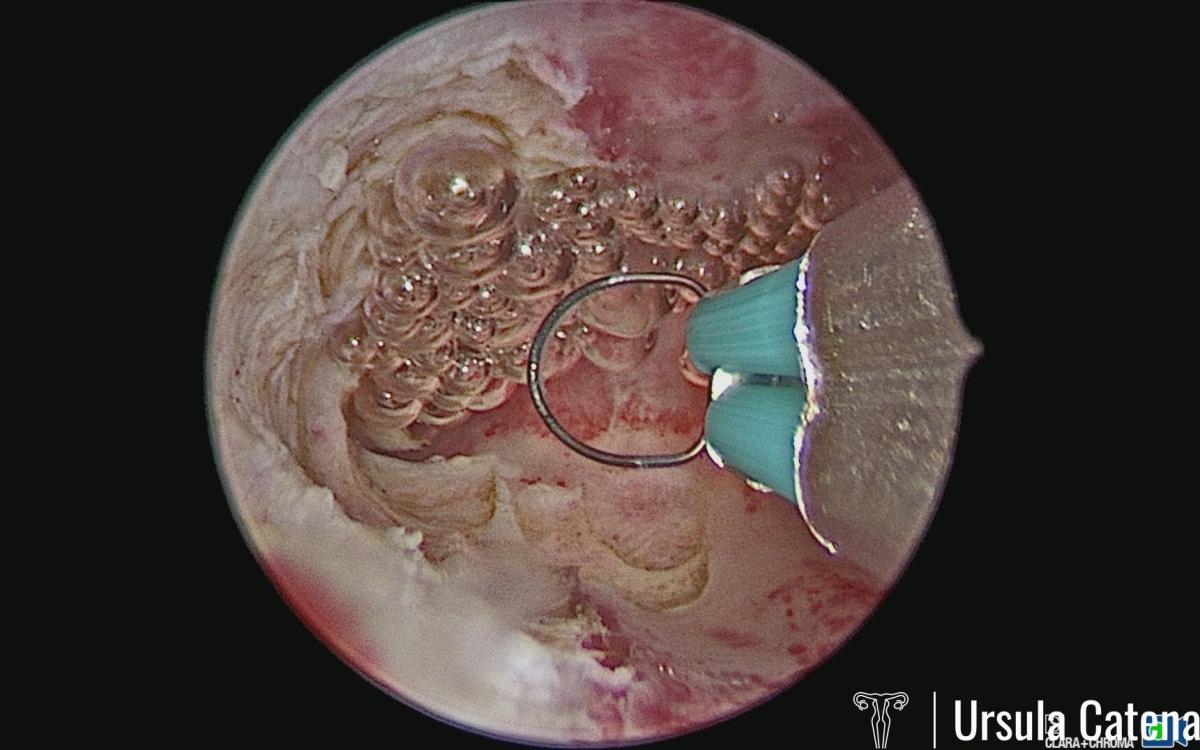
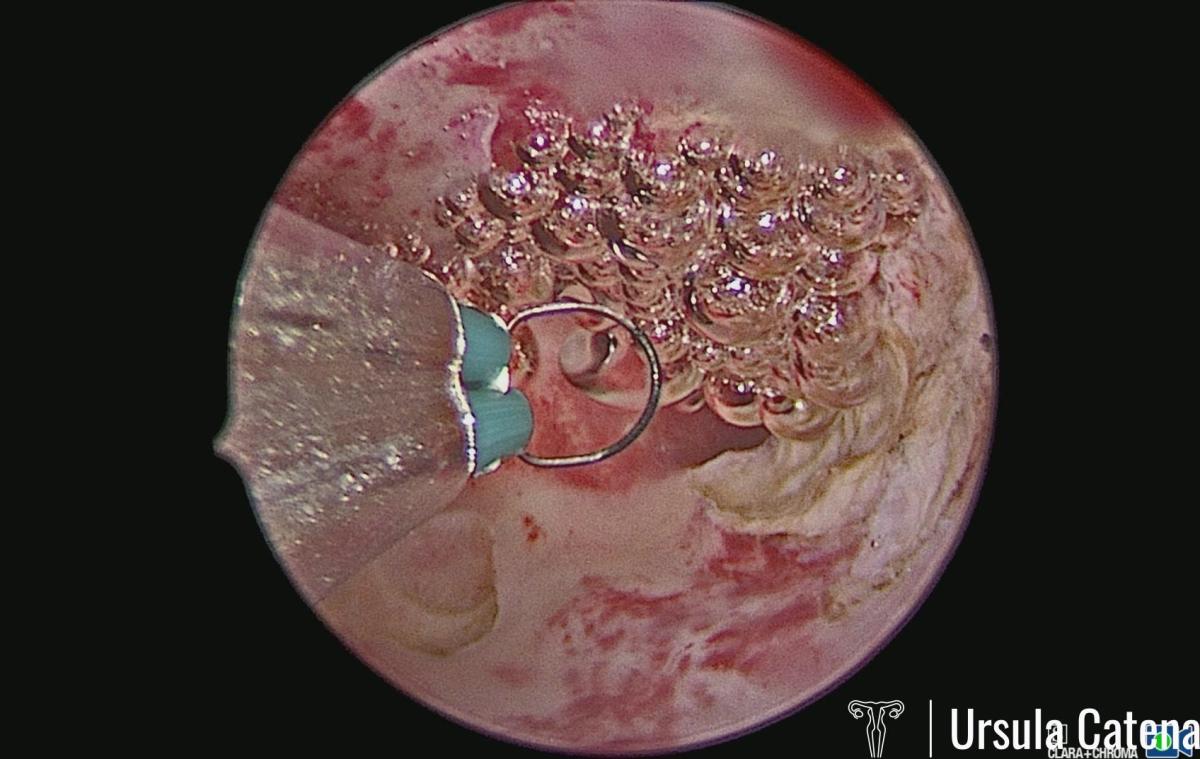
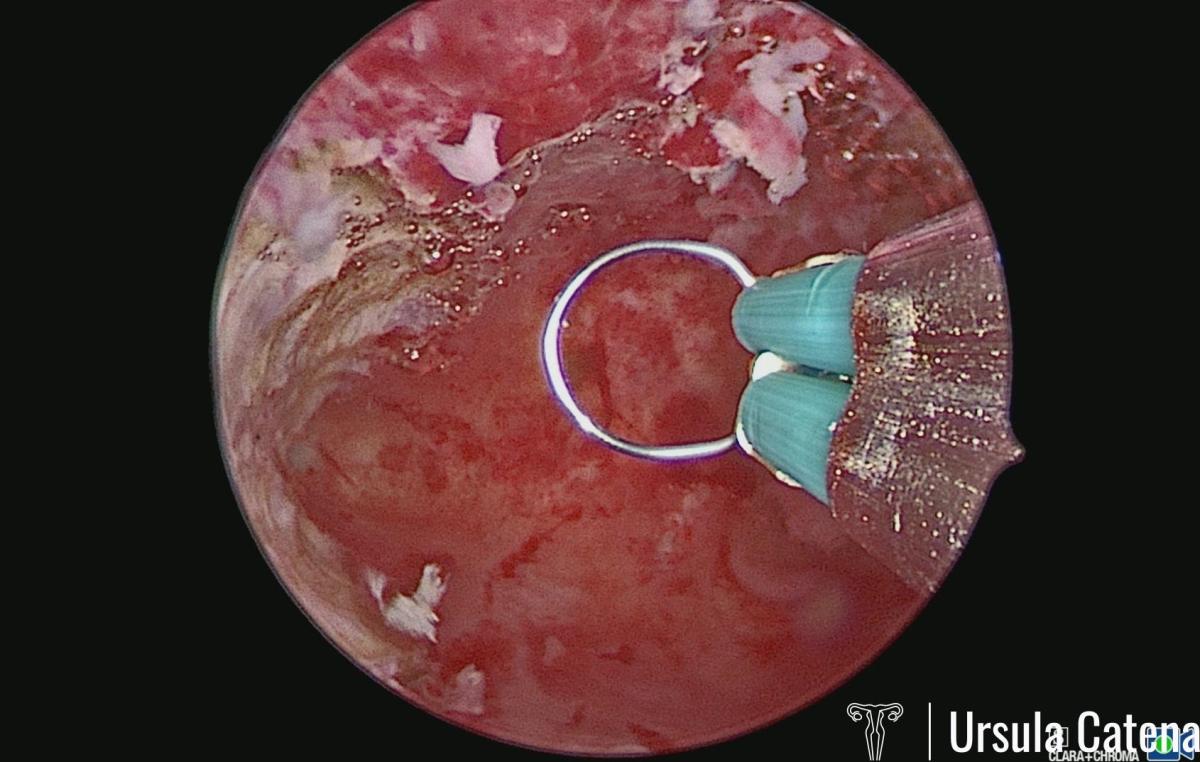
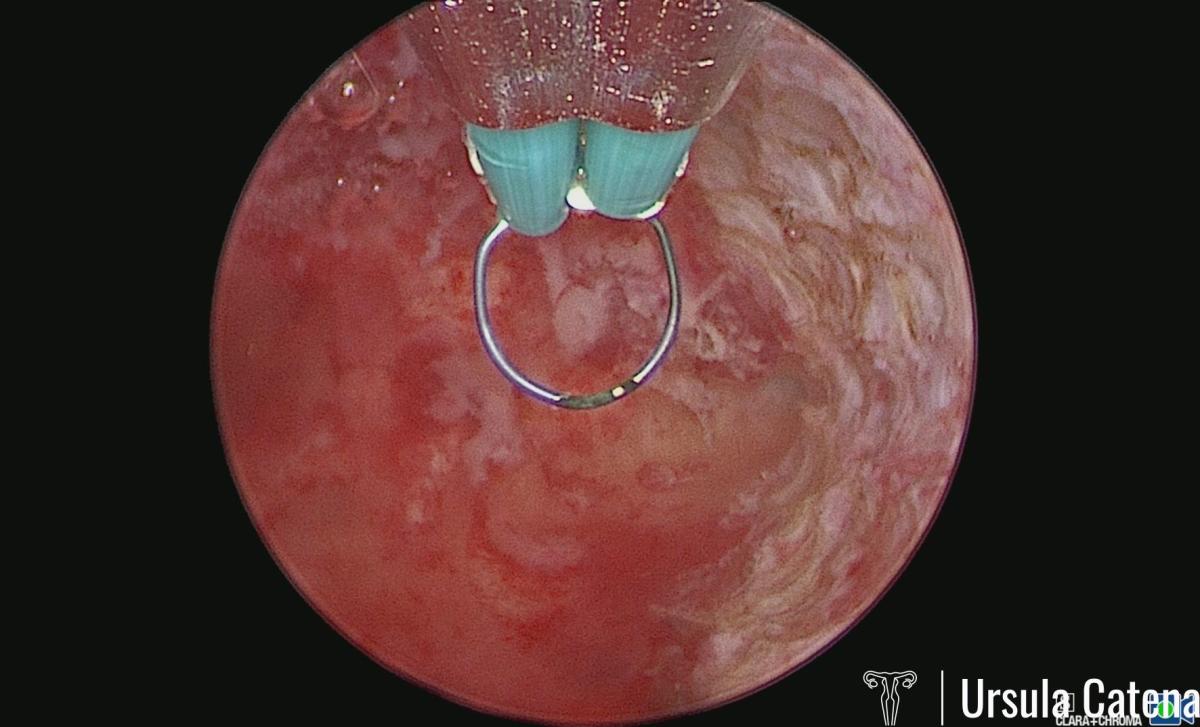
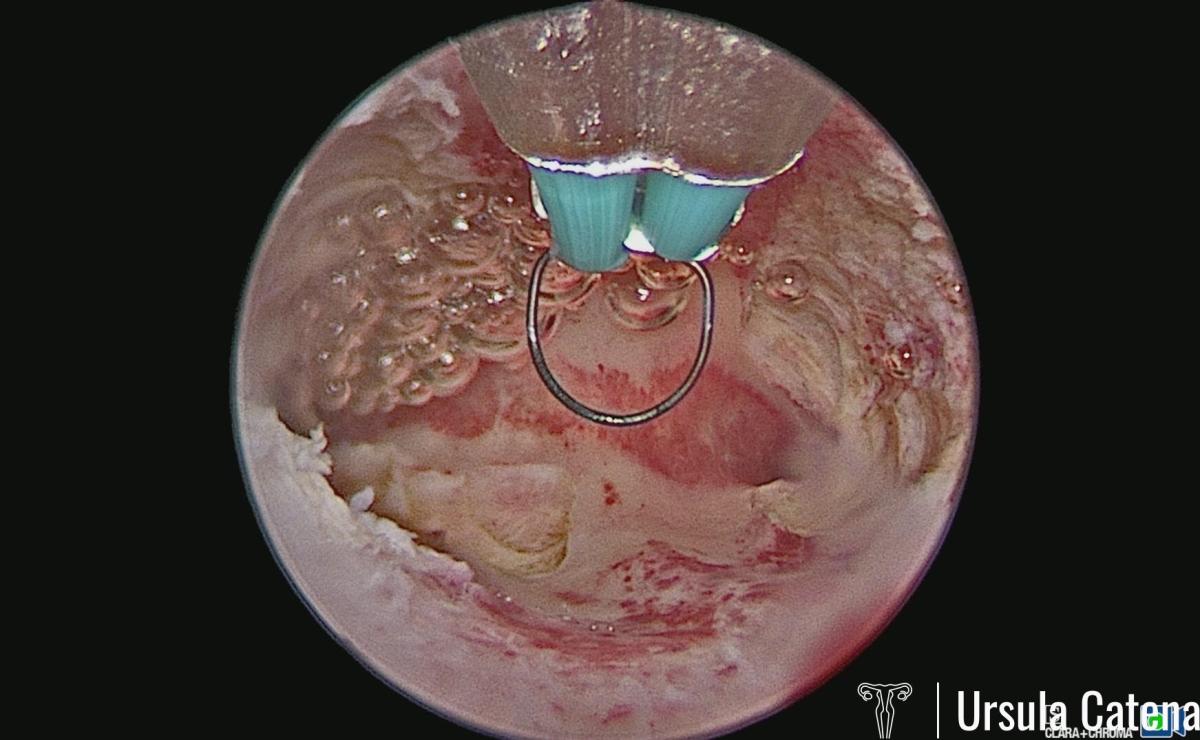
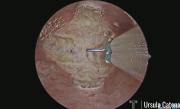
The hysteroscopic metroplasty procedure is performed under sedation and lasts about 20-30 minutes. At the CLASS Hysteroscopy center, metroplasty is performed with an innovative instrument, the 15Fr (5mm) bipolar miniresectoscope. The use of this miniaturized instrument allows us to avoid blind dilation of the cervical canal and to enter the uterine cavity without trauma to the cervix. The bipolar energy system allows a gentle cut with perfect tissue coagulation, avoiding the formation of intrauterine adhesions after the procedure. Before the procedure, a 3D ultrasound is performed which will confirm the pathology. The first surgical step consists in incising the septum with a Collins loop. Once a normal cavity has been recreated, it may be necessary to resect the abnormal tissue that remains at the level of the anterior and posterior uterine wall with a 90 ° loop. At the end of the procedure, haemostasis is checked, the success of the procedure is checked by 3D ultrasound and/or using an endoscopic graduated palpator and a hyaluronic acid gel applied to prevent adhesions.
In most cases, discharge occurs 3 hours after the procedure, without the need for hospitalization in an inpatient ward.
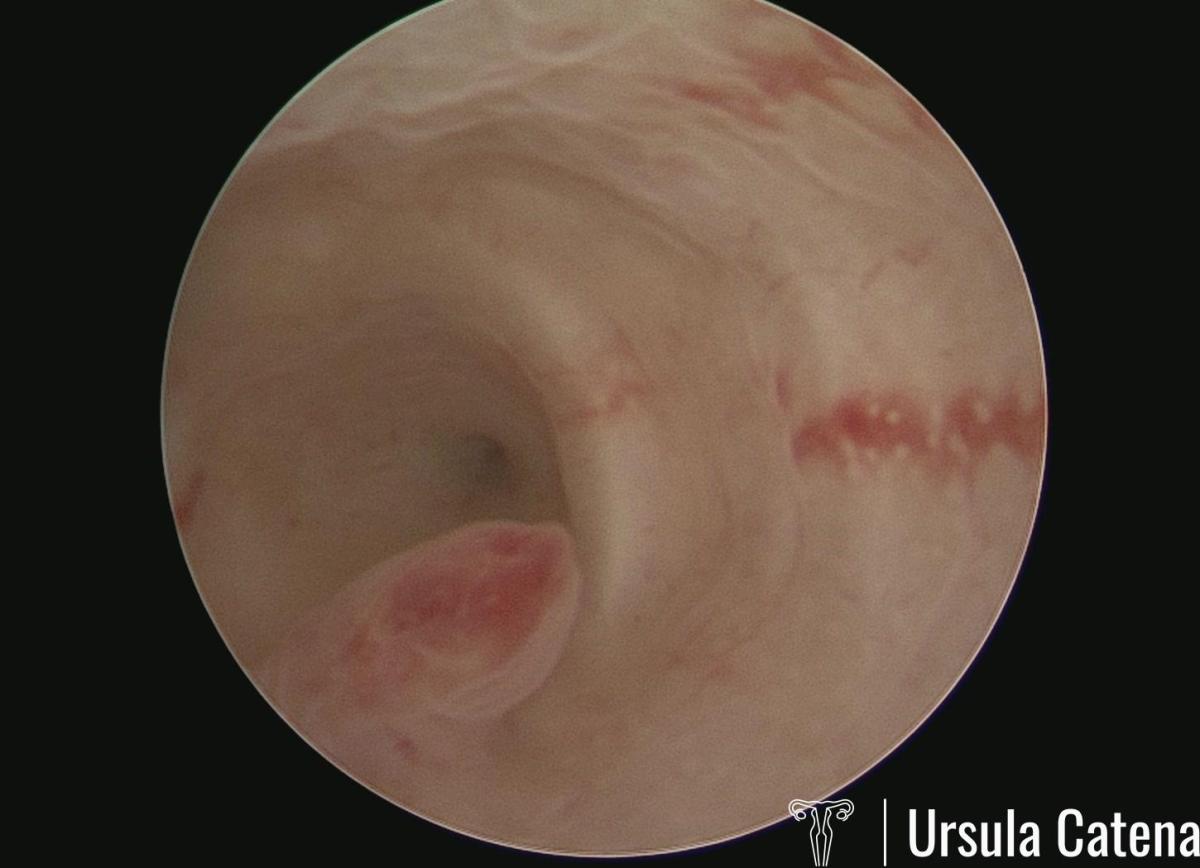
After 30-40 days from primary surgery, an office hysteroscopic control must always be performed: this prevents the formation of intrauterine adhesions and allows us to control the cavity. The uterine wall reshapes itself after the procedure, therefore it is normal, during the control, to find some little adhesions or a small residual septum at the fundus level; these findings can be managed with 5Fr miniaturized instruments during the office hysteroscopy itself.
The need for a second surgical step under sedation is infrequent in the case of an uterine septum; it may, on the other hand, be necessary in the case of surgery for complex uterine malformations. In most cases, after office hysteroscopic control, progestin therapy can be stopped, and the patient can seek pregnancy from the next menstrual cycle.
T-SHAPED UTERUS: DIAGNOSIS AND TREATMENT
The T-shaped uterus (or dysmorphic uterus) is a still little known anomaly of the uterus, which has been seen to be correlated with infertility and/or repeated miscarriages. Sometimes it appears to be the reason for the failure of assisted reproductive techniques, for the failure of implantation of the blastocyst in the uterus. In literature, a pregnancy rate of 73% is reported after hysteroscopic correction of this anomaly with 48% of pregnancies conceived spontaneously without resorting to assisted fertilization techniques; encouraging is the data showing that of these patients 32.5% had one or more previous failures of assisted reproductive techniques (Di Spiezio et al. 2019).
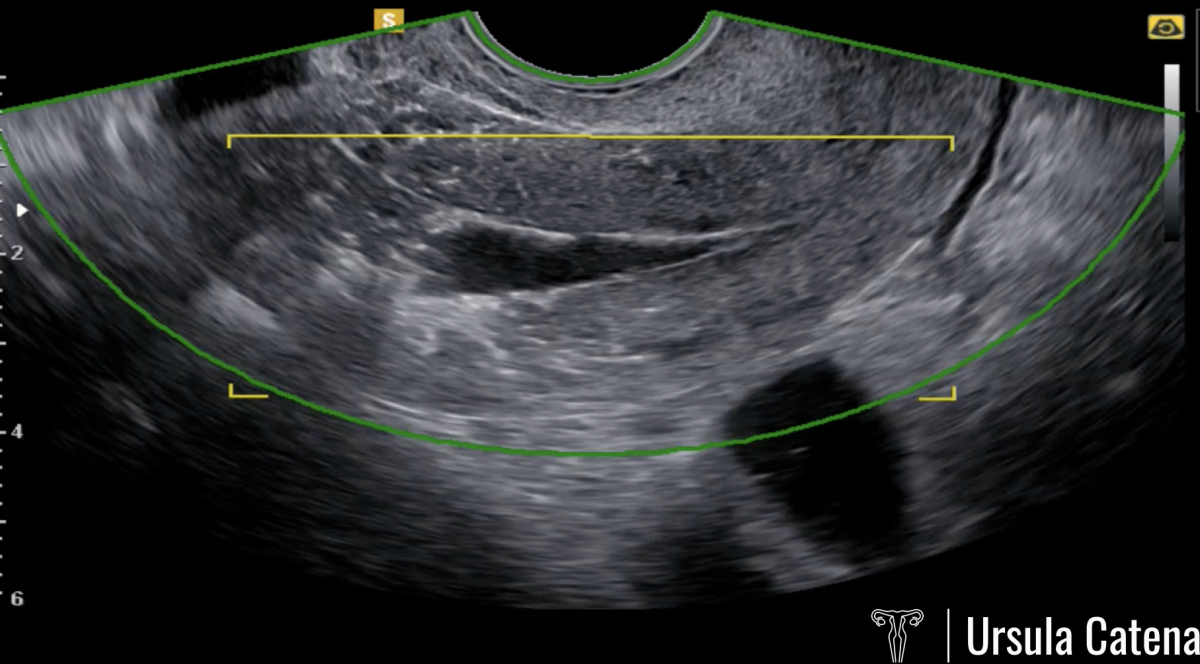
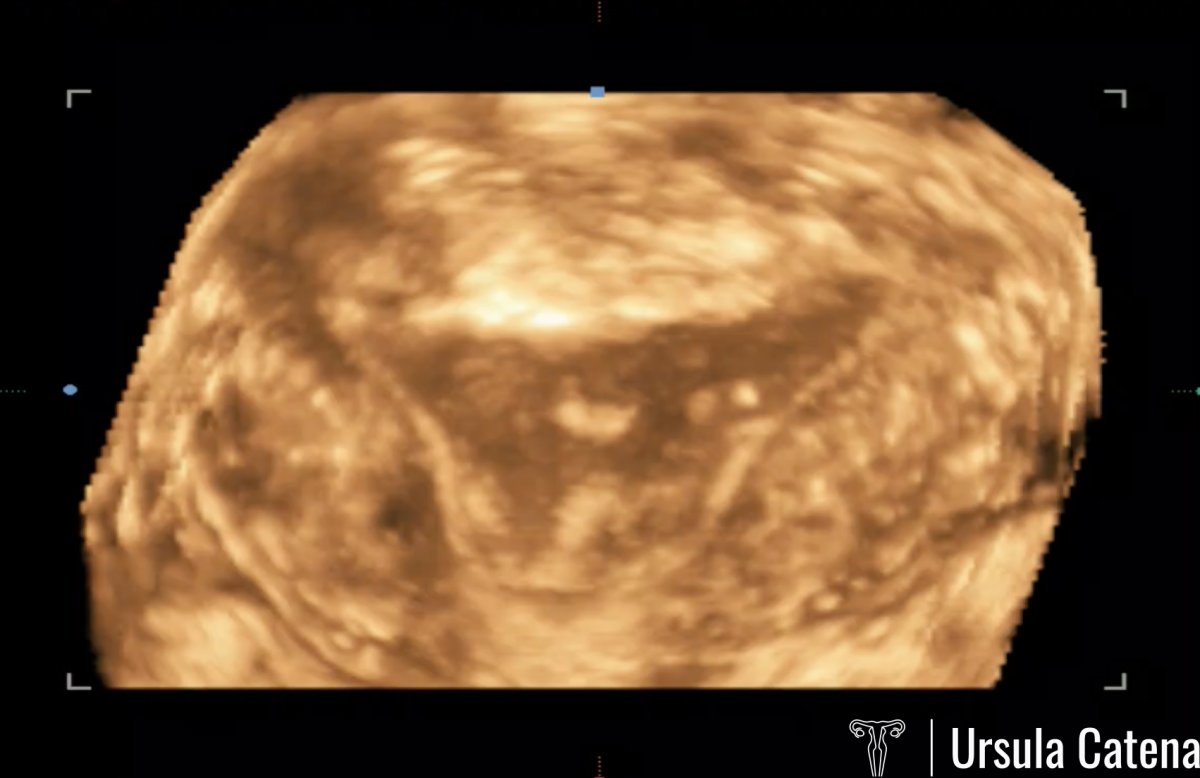
In the event of a suspected T-shaped uterus, at the CLASS Hysteroscopy center, patient first of all undergoes a 3D ultrasound and office diagnostic hysteroscopy.
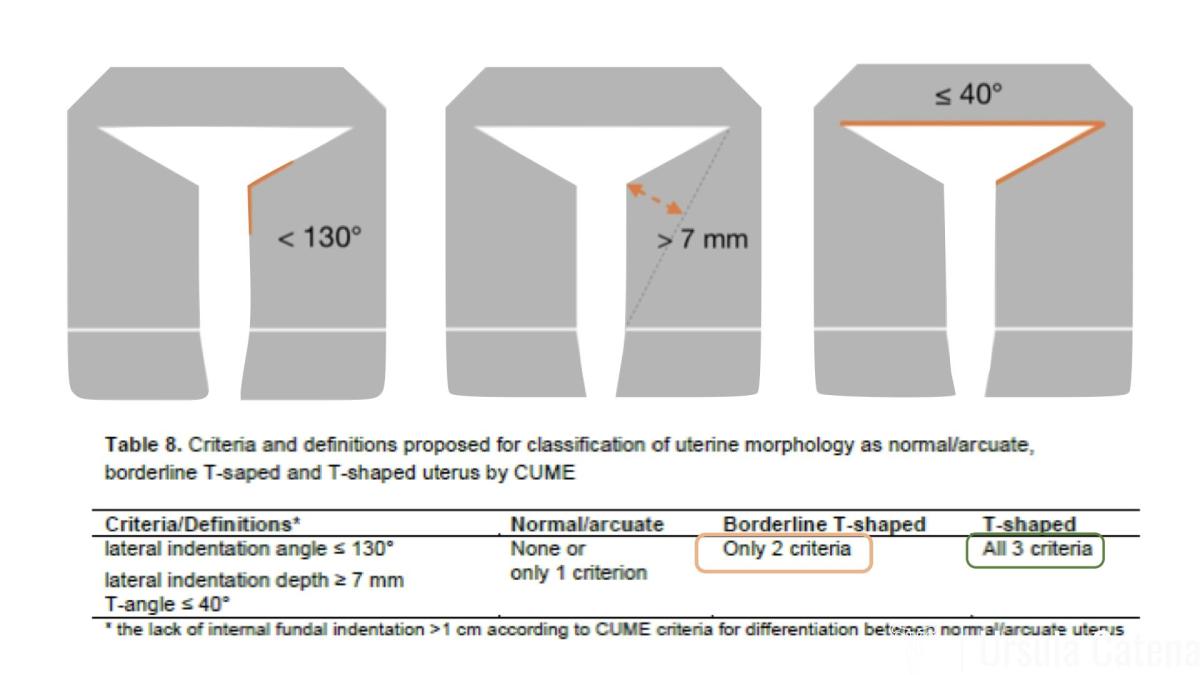
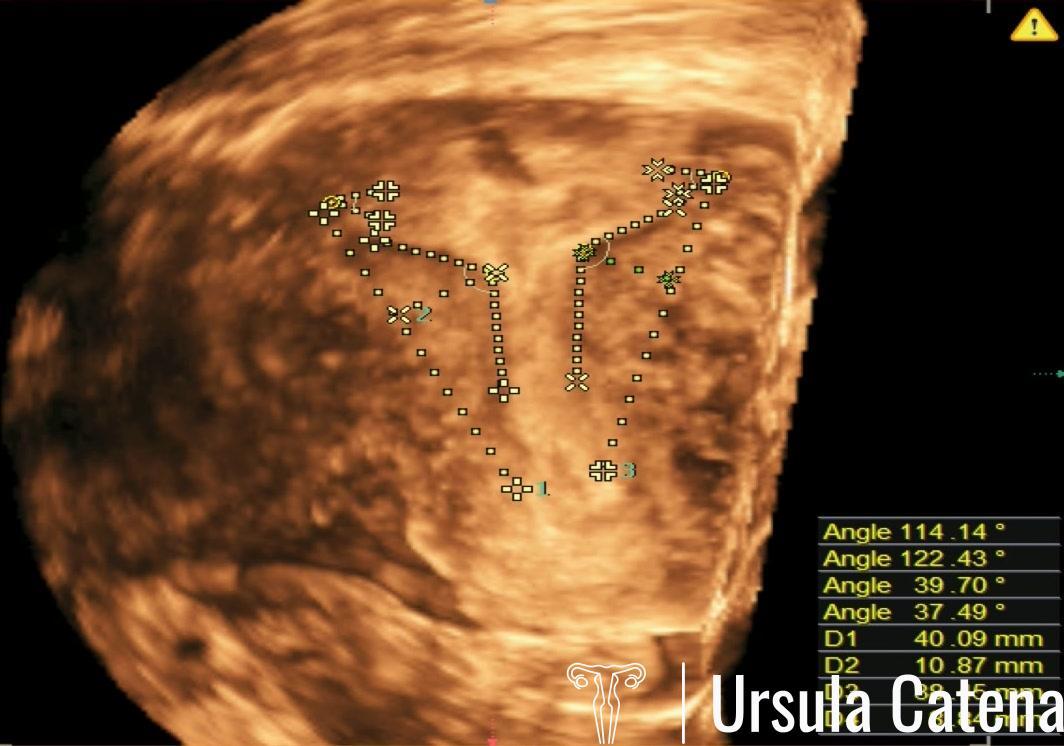
The 3D ultrasound examination is based on three diagnostic criteria established by the CUME (Congenital Uterine Malformation by Experts) Consensus: 1) lateral indentation angle ≤130 °; 2) side indentation thickness ≥7mm; 3) angle T ≤40 °.
Office diagnostic hysteroscopy will allow to confirm the ultrasound diagnosis.
Once the diagnosis of certainty has been reached and discussed with patient the therapeutic options based on her medical history (possible infertility and/or previous miscarriages), she will be advised to start oral therapy based on progestin or estrogen-progestin in order to prepare the endometrium for surgery. Therapy must be started from the first day of the next menstrual cycle and taken every day except for different indications from the doctor. The menstrual cycle may not occur and the onset of spotting (small blood loss) will be possible during therapy.
The hysteroscopic metroplasty procedure for dysmorphic uterus is performed under sedation and lasts about 20-30 minutes. At the CLASS Hysteroscopy center, metroplasty is performed with an innovative instrument, the 15Fr (5mm) bipolar miniresectoscope (Catena et al. 2021). The use of this miniaturized instrument allows us to avoid blind dilation of the cervical canal and to enter the uterine cavity without trauma to the cervix. The bipolar energy system allows a gentle cut with perfect tissue coagulation, avoiding the formation of intrauterine adhesions after the procedure. Before the procedure, a 3D ultrasound is performed which will confirm the picture. The first surgical step consists in incising the fibromuscular tissue of the uterine lateral walls with a Collins loop. Once a normal cavity has been recreated, it may be necessary to resect the abnormal redundant tissue that remains at the level of the uterine lateral walls with a 90 ° loop. At the end of the procedure, haemostasis is checked, the success of the procedure is checked by 3D ultrasound and a hyaluronic acid gel can be applied to prevent adhesions.
In most cases, discharge occurs 3 hours after the procedure, without the need for hospitalization in an inpatient ward.
After 30-40 days from primary surgery, an office hysteroscopic control must always be performed: this prevents the formation of intrauterine adhesions and allows to control the uterine cavity.
The need for a second surgical stage under sedation is infrequent in the case of a dysmorphic uterus. In most cases, after office hysteroscopic control, progestin therapy can be stopped and patient can seek pregnancy from the next menstrual cycle.
COMPLEX MALFORMATIONS: DIAGNOSIS AND TREATMENT
In case of complex malformations of the female genital tract, the treatment is tailored to the individual patient.
Sometimes an MRI scan is also needed for diagnosis.
The treatment of complex malformations does not always involve only an hysteroscopic approach, but sometimes it also requires a laparoscopic abdominal approach or, often, a combined approach. In these cases the procedure cannot be performed in one day surgery setting but an hospitalization in an inpatient ward for a few days must be planned.
Look our photos